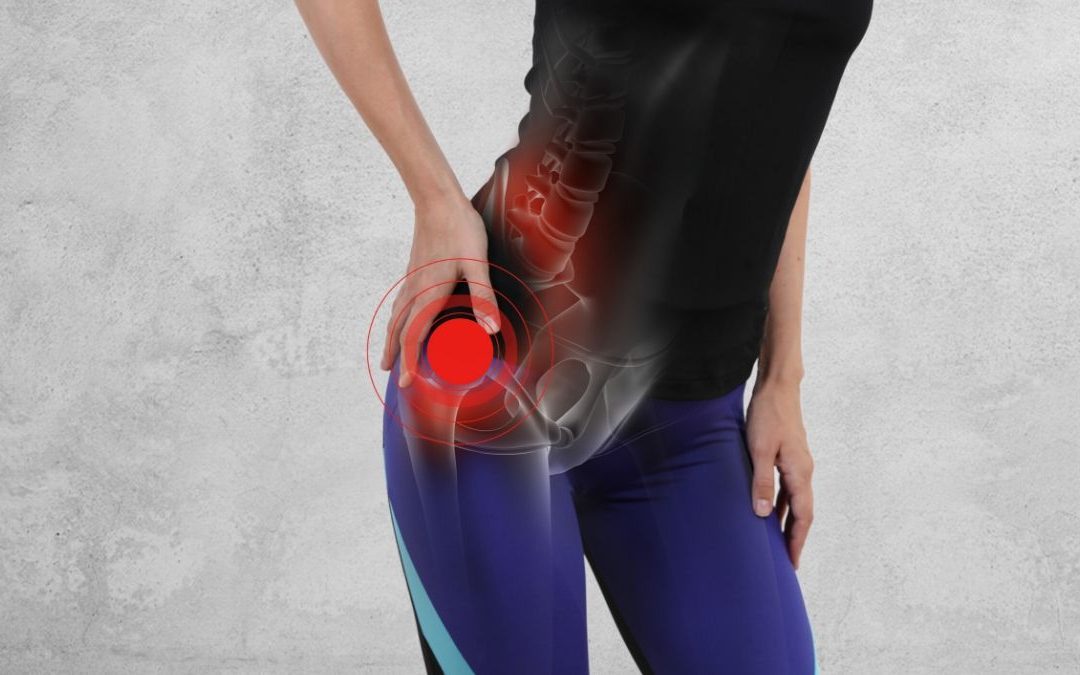
Lateral Hip Pain
We’re aware that normally the phrase is “What a pain in the Butt”, but in this instance, although we’re talking about one of your Butt muscles, it presents as “A Pain in the Hip”, well lateral hip at least. Today we are discussing lateral hip pain – which mostly commonly is a result of a Gluteus Medius Tendinopathy.
Gluteus Medius Tendinopathy is thought to be the primary cause of lateral hip pain presenting over the greater Trochanter (the bone on the outside of your hip) and extending down the outside of your thigh. Gluteus Medius Tendinopathy and Trochanteric Bursitis (an inflammation of the fluid filled sac that helps lubricate the space between the muscle tendons and bone) often exist together, however recent imaging studies have shown that approximately 80% of cases are attributed to Gluteal Tendinopathy, not purely as bursitis as previously thought.
Gluteus Medius Tendinopathy can be very painful and symptomatic, impacting a person’s ability to sleep, stand, walk, climb stairs, sit and exercise. It can significantly affect quality of life, ability to complete daily tasks and exercise tolerance.
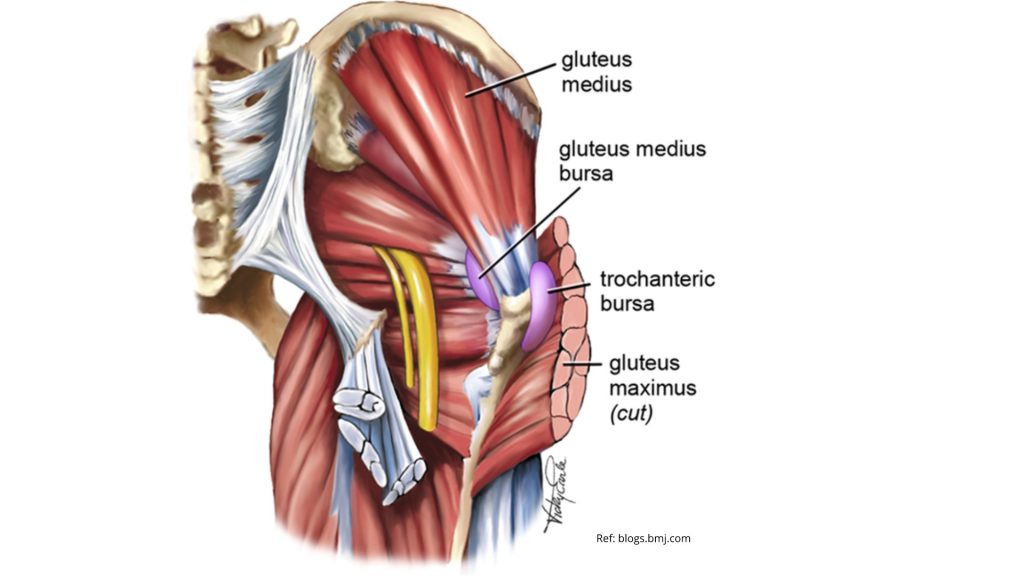
What is the Gluteus Medius?
The Gluteus Medius is one of the three gluteal or “butt” muscles. It is situated on the outer surface of the pelvis and its strong tendon attaches into the outside of the hip into a part of the thigh bone (femur) called the Greater Trochanter. The bursa separates the tendon of the muscle from the surface of the trochanter over which it glides. As a muscle Gluteus Medius has the main roles of abducting or bringing your hip away from your body, it helps to rotate the hip, and it has the important role of holding our pelvis stable when we stand on one leg – it prevents the opposite side of the pelvis from dropping during walking, running and single leg weight-bearing.
What is Gluteus Medius Tendinopathy?
Gluteus Medius Tendinopathy is traditionally thought of as an overuse injury caused by tensile or compressive loads beyond the capacity of the tendon ie your muscles tendon, can’t cope with the demands that you are placing on it. This can happen due to an increase in exercise, starting a new job, inadequate biomechanics, poor sitting/standing postures or repetitive aggravating tasks. Once aggravated, the tendon becomes highly sensitised making everyday tasks painful such as crossing legs, climbing stairs, lying on the side and walking. Without appropriate load management and strengthening, the tendon becomes more irritable, has reduced load capacity and an increased risk of developing a tear. In some cases Gluteus Medius Tendinopathy can also be caused by direct trauma such as a fall or from a previous muscle tear or injury.
What are the risk factors?
- Gender: it’s 4 times more common in females than males
- Age: Over 40 years old
- History of lower back pain
- Repetitive single leg weight bearing tasks
- Excessive stairs, low sitting and crossing legs
- Poor biomechanics and pelvic control
How do I find out if I have Gluteus Medius Tendinopathy?
Through a comprehensive Physiotherapy examination, we are able to diagnose Gluteus Medius Tendinopathy.
Although imaging can be useful in assisting the diagnosis of Gluteus Medius Tendinopathy, it should be used as an adjunct to examination as many individuals (up to 88%) can have signs of lateral hip pathology without pain according to Blankenbaker et al. (2008).
Best practice currently supports the use of a series of orthopaedic tests to diagnose patients with Gluteus Medius tendinopathy. Grimaldi et al. (2017) reports that these tests in combination with palpation by an experienced professional are as effective at identifying Gluteus Medius Tendinopathy as an MRI is. Once diagnosed correctly, a management plan can be formulated.
Should I rest and see, get a Cortisone Injection or start Physio?
Current evidence in the management of Gluteus Medius Tendinopathy involves a range of therapy options with research from Mellor et al. 2018 reporting that education plus exercise as well as a corticosteroid injection resulted in higher rates of patient reported improvement and lower pain than no treatment at eight weeks, but when measured alone, education plus exercise performed better than corticosteroid injection alone for long term improvement in pain and function. Brukner et al 2017 also report that cortisone injection may reduce pain in the short term, however the effect was not long lasting, indicating that targeted rehabilitation is warranted in order to get a great outcome.
How does Physiotherapy Treatment help?
Effective treatment of Gluteus Medius Tendinopathy relies on a combination of:
- The correct diagnosis,
- The identification & correction of biomechanical deficiencies
- Education on the condition
- The need to Address load management issues
- Modifying activities to reduce load and symptoms
- Completing a progressive strengthening program.

Physiotherapy helps patients with Gluteus Medius Tendinopathy using all of the above however the starting place is often with targeted soft tissue work to reduce muscular guarding due to pain and reduce compensatory muscular overactivity that occurs.
In the early stages, our physio’s will help by modifying aggravating activities and positions, and educating on load management, whilst starting to improve muscle activation patterns and biomechanics with targeted exercise.
Load management is particularly important in Gluteus Medius Tendinopathy with Cook et al (2011) recommending minimising positions of compression (side lying, crossed legs, adduction stretches) and controlling activities of high tensile loads (stairs, hill running).
Depending on the severity and duration of Gluteus Medius Tendinopathy, we then help to create a strong and healthy tendon by progressively loading it through exercise. Progressive loading allows the tendon to withstand different loads and forces such as tensile, stretching, compression, endurance (loading over time), explosive movement or a combination of all of these. It is important to understand that each of these types of loads is different and sits on a continuum from least stressful to most stressful i.e. lying on side = compression, squatting = stretching/tensile, running = combination of all forces.
By understanding these differing loads, our physiotherapists are able to then load the tendon in a way that is task specific and individualised. This ensures the tendon is able to withstand the different forces that are required for the differing demands of our patients. With this in mind, our Physiotherapists will help you safely get back to your chosen work, sport, exercise or life tasks that are affected, helping to reduce the risk of re-injury.
ARE YOU STRUGGLING WITH HIP PAIN?
GET AN ASSESSMENT & TREATMENT WITH OUR AMAZING TEAM OF PHYSIO’S.

- Get crystal clear about what’s causing your Hip Pain – is it Gluteus Medius Tendinopathy?
- Find out the most important steps for you to get pain free fast!
- Understand how to manage your load without suffering the consequences of hip pain
- Find out the simple yet essential exercises that can help you get lasting relief
- Leave the session with the confidence of knowing exactly what to do to get symptom free and back to living life without pain