Rotator cuff disease is prevalent in the general population, accounting for 10% of all shoulder pain and resulting in major shoulder disability (Abdulwahab et al, 2017). Shoulder pain is the third most common cause of musculoskeletal consultation in primary care (Mitchell et al, 2005).
The shoulder joint itself is classified as a ball and socket joint; and sacrifices stability for mobility, meaning it’s not as stable as some of our bodies joints as it moves so much! The joint gets its stability from static structures like ligaments, and the glenoid labrum; and more dynamic constraints like the Rotator Cuff (RC) muscles which keep us stable through movement.
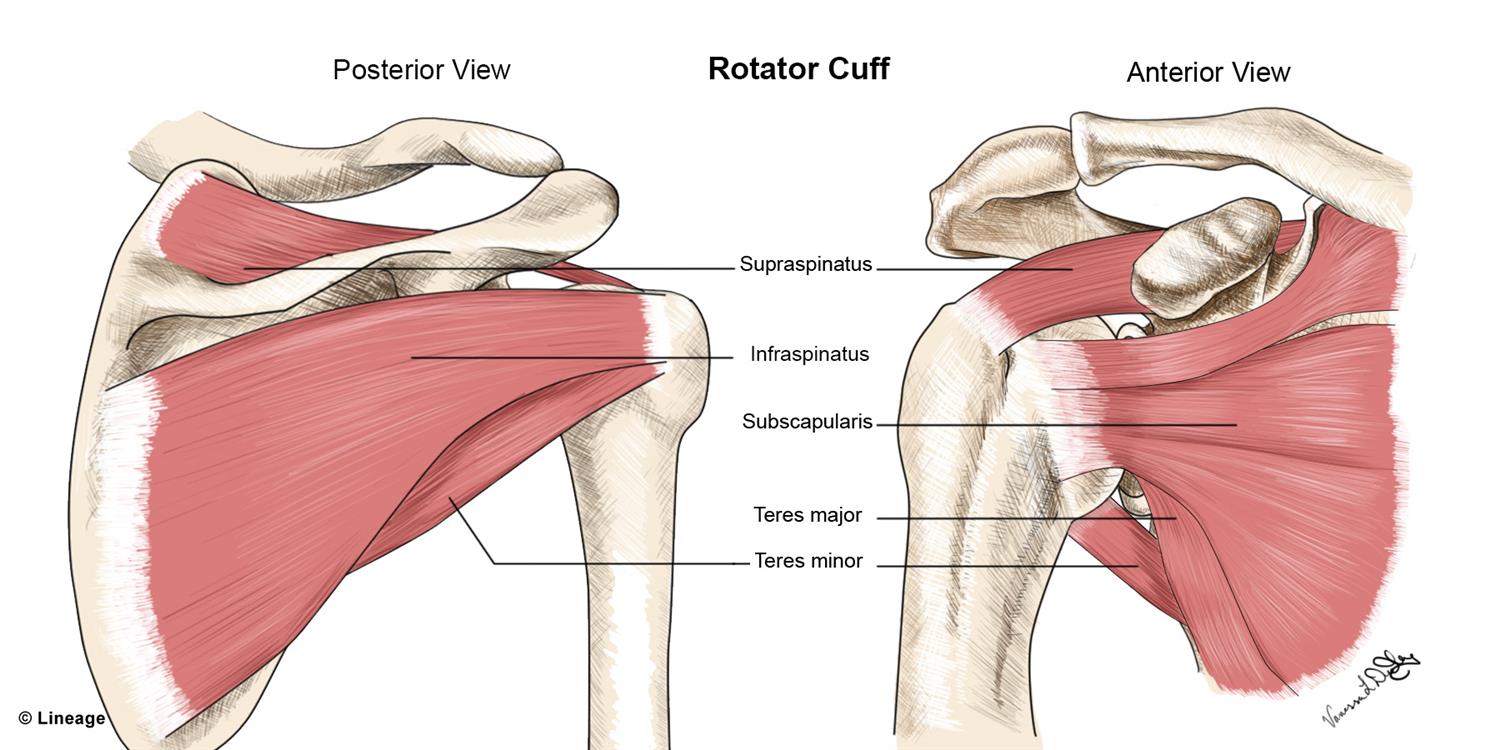
What is the Rotator Cuff?
The RC is comprised of 4 muscles and their tendons: Supraspinatus, Infraspinatus, Subscapularis and Teres Minor. These muscles all arise from the scapula or shoulder blade and connect into the head of the humerus or arm bone. They act in co-contraction (together as a team) to stabilise the humeral head (the ball) in the glenoid fossa (socket). Above the rotator cuff, there is a bursa which covers and protects the muscle and tendons, as they are in close contact to the surrounding bones.
The shoulder is the most mobile joint in the entire body making it easily susceptible to injury. Therefore, it requires a high degree of strength, stability and control which is provided by these RC muscles. Tears can either be traumatic or as a result of degeneration occurring in both sports people and the general public.
In a review by Mingawa et al. (2013) they found that the prevalence of rotator cuff tears in the general population is around 22%, which increased with age, and interestingly an asymptomatic tear (someone that had a tear but had no symptoms) was twice as common as a symptomatic or painful tear.
(https://step2.medbullets.com/orthopedics/120532/rotator-cuff-injury)
What causes the Rotator Cuff to tear?
Rotator cuff tears can be separated into two categories:
Traumatic: A one off incident as a result of a fall or external force. This can be associated with a weakened or fatigued muscle being overloaded, leading to a tendon rupture.
Degenerative: A result of gradual degeneration of the tendon due to overuse, poor biomechanics and age. These tears can have an insidious onset of pain and are usually exacerbated by movement. Rotator cuff tendinopathy often proceeds a tear as it is associated with tendon degeneration creating pain and weakness.
Brukner and Khan (2017) suggest that if identified early enough, physiotherapy can help to treat rotator cuff tendinopathy and impingement prior to it developing into an overuse degenerative RC tear.
Who is at risk of rotator cuff pathology?
The incidence of rotator cuff tears increases with age, with full-thickness rotator cuff tears present in approximately 25% of individuals in their sixties, and more than 50% of those in their eighties (Edwards et al. 2016).
Other risk factors include:
- Those who participate in contact and throwing sports
- Overuse or repetitious above head tasks
- A history of shoulder arthritis
- Poor biomechanics – including lower kinetic chain dysfunction

How are symptoms of RC pathology described?
Importantly, RC tears or injuries are not always associated with pain or patient-reported loss of function (Bachasson et al. 2015). It is worth noting that asymptomatic patients may develop symptoms in a relatively short period of time.
The most common signs of rotator cuff injuries are:
- Painat rest and at night, particularly if lying on the affected side.
- Painwhen lifting and lowering the arm or with reaching.
- Pain during ADL’s like dressing, doing hair and domestic activities such as scrubbing and hanging laundry.
- Weaknesswhen lifting or rotating the arm.
Diagnosis and examination:
Physiotherapy plays an important role in diagnosing RC tears and also where necessary, determining who requires a referral for appropriate imaging and specialist opinion.
Diagnosis is achieved through a comprehensive subjective examination understanding the mechanism of symptoms or injury, and determining lifestyle factors that may be impacting symptoms, but then also via clinical testing during an objective examination.
Typical findings on clinical assessment include:
- Pain typically localized to front and outside of the shoulder, and may refer down the outside of the upper arm.
- Painful & restricted range of motion when lifting above head and behind back
- Muscle weakness & pain on muscle testing and special tests
- Functional impairments: difficulty lifting, pushing, reaching, overhead movements and moving the hand behind the back like doing up one’s bra.
- Scapular (shoulder blade) Dysfunction. Studies of patients with rotator cuff tears have shown increased scapular upward rotation of some magnitude (Kibler et al. 2013).
- Kinetic chain dysfunction (the way body works together to produce force) is also often noted in patients with shoulder pathology. On assessment, 70% of the population will exhibit a connection to the opposite lower limb, while 30% of the population will have a connection to the same side, meaning that if there is dysfunction in the lower limb it can affect the forces transferred into the shoulder causing pathology. Interestingly, up to 80% of the power required to throw comes from the lower body (Wilk (2016), Chalmers (2017), Ellenbecker (2020), Laudner (2019)). This research links the importance of core and gluteal stability in order to transfer force to the shoulder.
Physiotherapy examination also helps to differentiate shoulder pain that may originate from sources other than the shoulder, such as the neck (referred cervical or thoracic pain) or elbow, and also pain from other structures in the shoulder, such as the labrum or joint itself.
RC muscles cannot be seen on X-rays but calcifications, arthritis or bony changes – that are common causes for rotator cuff pathologies – may be visible. The most common and accurate imaging method to evaluate rotator cuff pathologies is MRI. It can detect tears and inflammation and may help to determine size and character of the tear in order to establish what appropriate treatment might look like. Although MRI is the gold standard imaging method for rotator cuff pathologies, diagnostic ultrasound can also be used as it has a good diagnostic accuracy in the hands of a good sonographer, so can be more cost effective and readily available.

How does Physiotherapy help?
Once a tear is confirmed, a decision regarding conservative or surgical management needs to be made based on the severity of the tear, age of the patient, and their functional and sporting requirements and goals. Physiotherapy aims to achieve full range of motion, improvement of scapular control and restoration of strength, motor control and flexibility with a graded return to full activities/sport/function. Kibler et al. (2017) breaks down treatment interventions into five main areas: shoulder flexibility, pelvic and core strengthening, scapular control, and RC activation.
Manual therapy such as soft tissue massage, active releases and joint mobilisations is superior in improving range of motion when added to exercise compared to exercise alone (Steuri et al. 2017). Biomechanical analysis can identify dysfunction, abnormalities or compensations contributing to shoulder pain and thus guide the prescription of exercises. At Five Dock Physiotherapy & Sports Injury Centre we provide both manual therapy when indicated alongside individualised and progressive exercise programs for our patients that focus on improving strength, endurance and motor control through full shoulder motion taking into consideration scapular mechanics and the kinetic chain to achieve optimal results. Kinetic chain exercises may include lower limb strengthening, core and gluteal exercises and mobility work to improve thoracic, cervical, or lumbar ROM and often progress to functional and task specific exercises. The impacts of posture, education around its impacts and postural retraining exercises are also included where needed.
In our clinic we also use the AxIT system as part of our management. The AxIT system uses force plates and dynamometers to assess strength, endurance and power of specific muscle groups. It assesses muscle force production patterns during functional movements and can analyse specific exercises. It allows us to identify muscle imbalances side to side in the rotator cuff and also analyse the body’s ability to produce force by testing other areas in the kinetic chain. This data can help guide our patients during conservative management or post-op rehab giving them realistic measures and goals to achieve as they return to function.

Surgical vs Conservative Management of rotator cuff pathology
Historically partial RC tears have been treated with surgical repair and subsequent rehabilitation due to the inability of the tendon to repair independently. There is however recent evidence advocating for conservative treatment as the initial modality with Ryosa et al. (2017) demonstrating surgery is not more effective than conservative rehabilitation alone in partial thickness tears. Jeanfavre et al. (2018) further emphasised the benefit of exercise therapy with pain, range of motion, strength and function improving in greater than 80% of participants, with only 15% of RC tears transitioning to surgery. Abdulwahab et al. (2017) reported “a conservative treatment program is a reasonable approach within the first 6–12 weeks in patients with non-traumatic tears. If the patient does not respond within the initial 4–6 weeks, then it can be an indicator for transition to surgical treatment.”
If, however, the RC tear is moderate to large or the functional deficit is significant then surgery may be required more urgently. The most common rotator cuff muscle that is torn is the supraspinatus tendon and it is normally repaired via arthroscopy. Following surgery there is typically a period of immobilisation before post-op physiotherapy and rehabilitation can begin guided by the surgeon’s protocol. Thomson et al. (2016) conducted a study into post surgical protocols and found that post surgical improvements were achieved consistently across varying rehab protocols. Khatri et al (2019) via meta-analysis demonstrated both surgical and non-surgical treatment groups had the largest improvement at 12 months, so unfortunately those suffering need to be patient but also found that there was no clear advantage of surgery over non-surgical treatments.
Conclusion
Rotator cuff tears can be a debilitating and life changing occurrence. Our physiotherapy practice plays an integral role in recovery to assist with range of motion, strength and return to sport or everyday function, whether the tear is being treated conservatively or surgically. Although there is consistent evidence supporting rehabilitation and demonstrating the potential for physiotherapy to both improve shoulder outcomes and avoid surgical intervention, some patients will require surgery for the best outcome. Although this being said, physiotherapy is a great first step for many patients suffering with shoulder pain as physio not only helps to reduce symptoms and improve function, but diagnostically physio’s are experts in assessing shoulders and determining who may respond better to conservative management and which patients need a more urgent orthopaedic referral.
If you have shoulder pain and you are concerned that it could be a Rotator Cuff Tear, then it’s probably worth your while getting an assessment by our team of professional physiotherapists.