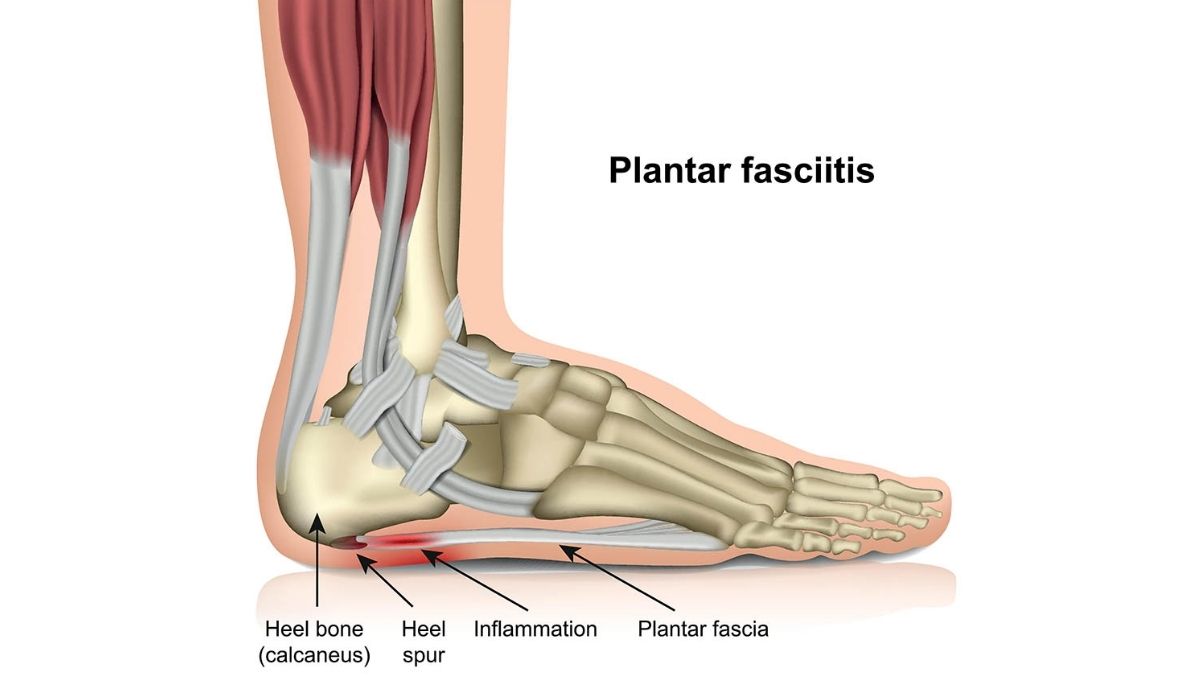
Plantar fasciopathy (PF) is one of the most common causes of heel pain.
It involves inflammation of a thick band of tissue that runs across the bottom of your foot and connects your heel bone to your toes (plantar fascia).
Signs and Symptoms
- Pain with first steps in morning
- Increase in training load
- Change in type of training
- Recent change in footwear
- Prolonged standing
- Pain localised at the bottom of your heel
- Onset is gradual
Plantar Fasciopathy has an estimated prevalence of 3.6-7% and is the most common cause of inferior heel pain.
Risk Factors
- Ages 45-60 are at a higher risk.
-
Increase intraining/exercise load.
- Recurrent periods of prolonged standing.
-
Poor biomechanics (e.g. Varus/bowed knees, poor gluteal/pelvic stability).
- Pregnancy, overweight & inactivity.
Diagnosis
- Pain on assessment of functional plantar flexion such as single leg calf raise (raising up on toes on one leg).
- Tenderness over the origin of the plantar fascia, medial ankle and fat pad. This can be located to the inside and bottom of the heel.

- Restricted range of motion through the ankle, and restricted big toe extension.
- The diagnosis is confirmed with a positive “Windlass test”.

- During the assessment, the physiotherapist will examine the muscle activation patterns & biomechanics of the lower body to determine the cause of the excessive loading on the plantar fascia.

Early diagnosis and management will lead to an improved prognosis and will allow a quicker return to activity.
Management
Conservative management is currently the treatment modality of choice for plantar fasciaopathy (Monteaguado, 2018, Berbrayer & Fredericson, 2014). This will comprise of:
- Education about pathology and prognosis to reduce level of threat.
-
Soft tissue massage, manual therapy, stretches and self-release exercises like spikey ball use or self massage with an iced water bottle.

- Load Management – this means adjusting the patients’ time on their feet, their training schedule or workload & systematically “re-loading” with exercise.
- An exercise program addressing biomechanical issues in the lower body such as gluteal and core dysfuction.
-
Footwear advice
-
Strength training and improving endurance of the intrinsic foot muscles, tibialis posterior and calf muscles.
-
Reduction of aggravating activities such as running or prolonged standing.
- Adjuncts such as taping, heel cups, and orthotics where indicated.

Evidence
- Caratun et al (2018), used a 3-month strengthening program, stressing the plantar fascia through progressive concentric and eccentric resistance exercises (using the windlass mechanism with Achilles tendon loading).
- Strength programs were found to have an improvement in foot function, with reduced disability and pain three months following the strengthening program (Rathleff et al, 2014 & Caratun et al, 2018).
- McPoil et.al 2019 found that a stretching and strengthening program in conjunction with shoe inserts proved beneficial in the management of PF, whilst also suggesting the importance of including hip strengthening including gluteal and pelvic stability exercises in the holistic management of PF.
When Should Physio Start
If you or someone you know is suffering from:
- Morning heel pain getting worse
- Pain is impacting your daily actvities
- Struggling to run
- Heel pain is starting to affect work
GET AN ASSESSMENT & TREATMENT WITH OUR AMAZING TEAM OF PHYSIO’S.
- Get crystal clear about what’s causing your injury or pain
- Understand what activities you can do without suffering consequences of pain or instability
- Find out the simple yet essential exercises that can help you achieve amazing result
- Leave the session with the confidence of knowing exactly what to do to get symptom free and back to living life to the full

