Patella dislocations are a common musculoskeletal injury accounting for approximately 2 to 3% of all knee injuries (Atkin et al., 2020). A patella dislocation occurs when the kneecap (patella) completely moves out of its normal place in the trochlear joint groove at the end of the femur (thigh bone) typically shifting in a lateral direction (outside of knee). The patella can either dislocate (completely pop out of this groove), or partially dislocate, known as a patella subluxation. Typically, a patella dislocation is paired with a rupture or high-grade tear of the Medial Patellofemoral Ligament (MPFL). The MPFL provides 50-80% of the structural support that opposes or counteracts the lateral
gliding (outward) movement of the patella (Brukner, 2018). With a subluxation, the patella can partially move out of its groove, and also relocate naturally. This may be a result of a non-complete tear of the MPFL or may also occur when people have ligamentous laxity or “stretchy ligaments”. The recurrence rate following a first-time dislocation can be as high as 15-60% (Hayat et al., 2020).
Risk Factors / Causes
- The anatomy of an individual’s knee can predispose them to dislocation.
- Generalised ligamentous laxity/hypermobility.
- Can be relatively increased due to hormonal. fluctuations during the menstrual cycle in females .
- Females: higher risk due to increased Q angle.
- Biomechanical: Muscle imbalance/poor activation/strength.
- The Vastus Medialis Oblique (quadricep muscle) acts as a dynamic stabiliser pulling the patella medially (inwards). It it’s not working effectively subluxation and dislocation can be more common.
- If the gluteus medius muscle of the hip isn’t working effectively this can lead to increased valgus buckling of the knee (inwards) compromising patella tracking.
- Excessive weight/obesity.
- 15-60% recurrence rate after first dislocation if not surgically managed.
How does a patella dislocation occur?
Patella dislocations typically occur in non-contact mechanisms but can arise following direct contact trauma. Non-contact patella dislocations typically occur when the knee is simultaneously flexed and in a valgus position (bent in) (Tsai et al., 2012), primarily when changing direction, side stepping or landing from a jump.
Lateral dislocations that occur as a result of direct trauma are often caused by a direct blow to knee. Less commonly a medial dislocation can occur with a blow to the lateral side of knee and this often occurs due to previous patellofemoral instability. (McCarthy et al, 2015)
Diagnosis and Examination
The patient usually complains that the knee gave way suddenly while twisting or jumping. Patients often describe the feeling of something moving or popping out. The dislocated patella will usually relocate spontaneously with knee extension, however in severe cases the patient may need to have a nerve block and medical assistance.
Patients typically present to the clinic with a large intracapsular effusion, an inability to extend their knee coupled with an antalgic gait or inability to weight bear. Clinically the patella apprehension test is positive.
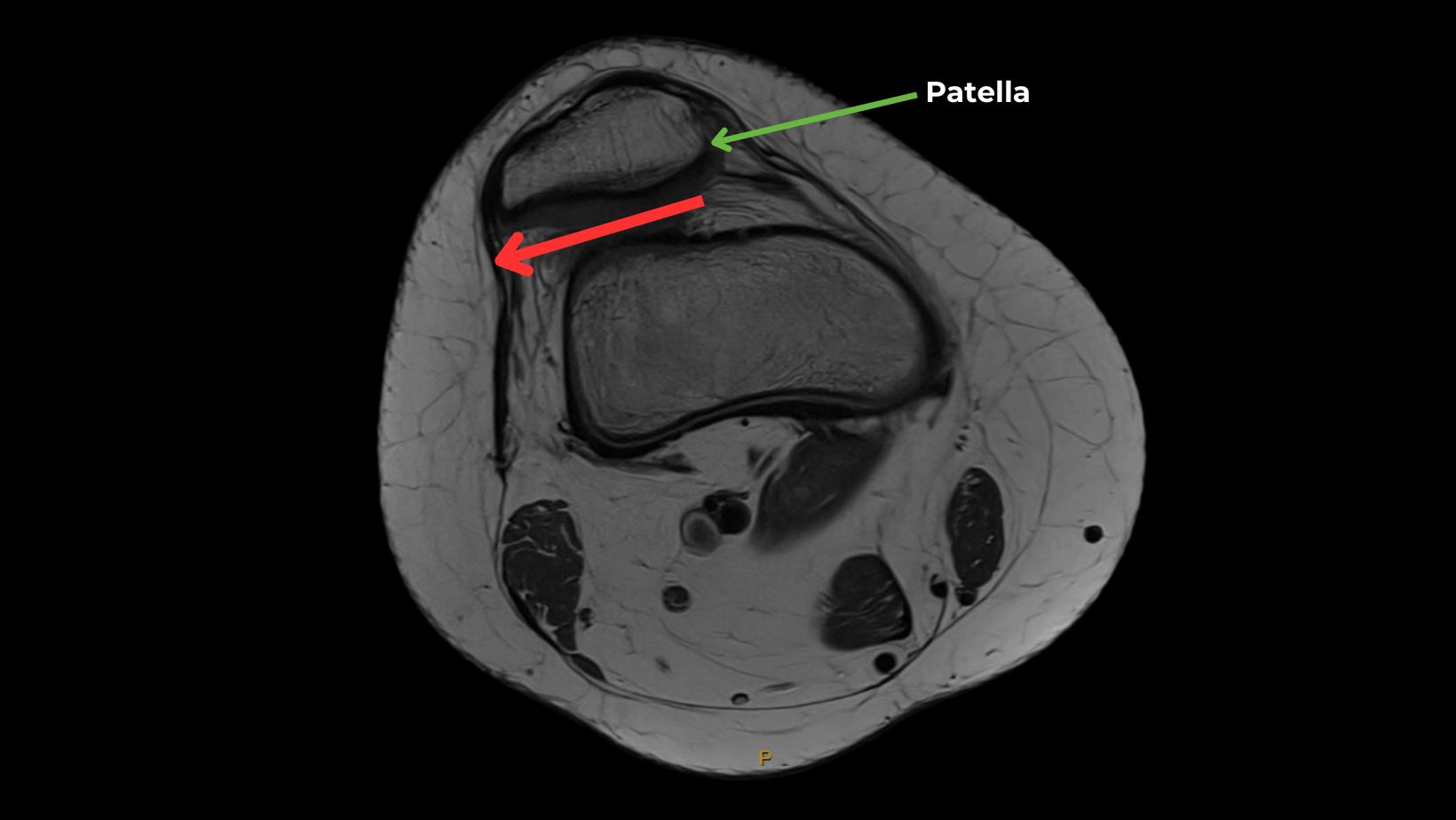
Imaging is often required to help diagnose the extent of the damage to the structures within the knee. An X-ray can help determine the possibility of a patella fracture. An MRI will confirm the presence of the MPFL being torn, probable retinacular injury, bone bruising and also help rule out the presence of other injuries such as ACL, PCL, MCL, meniscal tears or fat pad irritation.

Management
Patella dislocations can be treated both surgically and non-surgically, depending on individual factors.
Conservative management is the most common form of treatment after a patient’s first patella dislocation except in specific circumstances:
- Presence of an osteochondral fracture
- Substantial disruption of medial patella stabilisers
- Laterally subluxated patella with normal alignment of contralateral knee
- Second dislocation
- In patients not improving with appropriate rehabilitation
Following an acute dislocation, an X-ray & MRI will be arranged and then where necessary an orthopaedic surgeon’s opinion will be sought. A ROM brace and crutches are typically provided.
Rehabilitation for a patella subluxation or dislocation can start at day 1 once a fracture is cleared. This is typically in the form of VMO activation exercises, gentle stretches, manual therapy /soft tissue work, cryotherapy, compression and advice regarding knee protection and weight bearing.
Physio rehabilitation whether conservative or post-operative will often follow a similar path. Initially physiotherapy focuses on protecting the area, reducing swelling and promoting VMO muscle activation. From there we focus on restoring normal gait, improving ancillary muscle strength and activation (core, hip and calf) and then regaining range of motion of the knee. There is a particular focus on quadriceps strengthening, and specifically VMO training as it acts as a dynamic stabiliser of the patella, holding it medially. Rehabilitation also targets the muscles up and down the kinetic chain and as total leg strength improves more dynamic movements such as simple hopping and jumping will commence and an agility program can begin prescribed by the physiotherapist consisting of plyometric work, change of direction and a progressive running/sprinting program. This ultimately leads towards a safe return to training and sport. As a return to normal activities of daily living occurs both taping and a functional J brace can assist with control of the patella and improve a patient’s confidence in the knee. The most important aim of rehabilitation after a patella dislocation is to reduce the chances of a recurrent injury and to facilitate a safe return to normal activity and sport.

Exercise
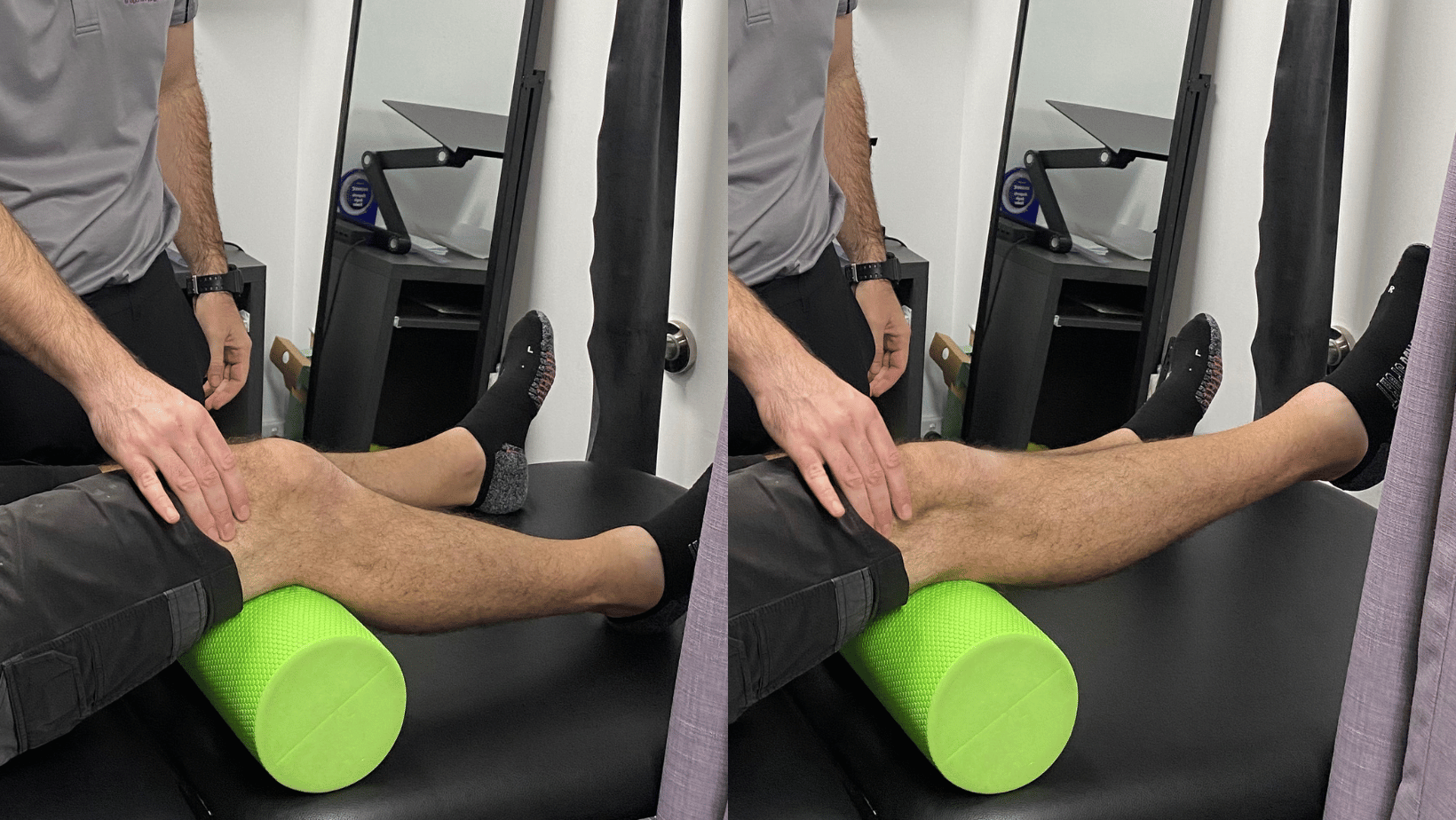
Inner Range Quad
Aim: Improve quadriceps and VMO strength and activation.
How: Place a rolled up towel or a foam roller under your knee. Extend your knee kicking out activating your quadriceps muscles and VMO. Hold for 5 seconds and repeat for reps.
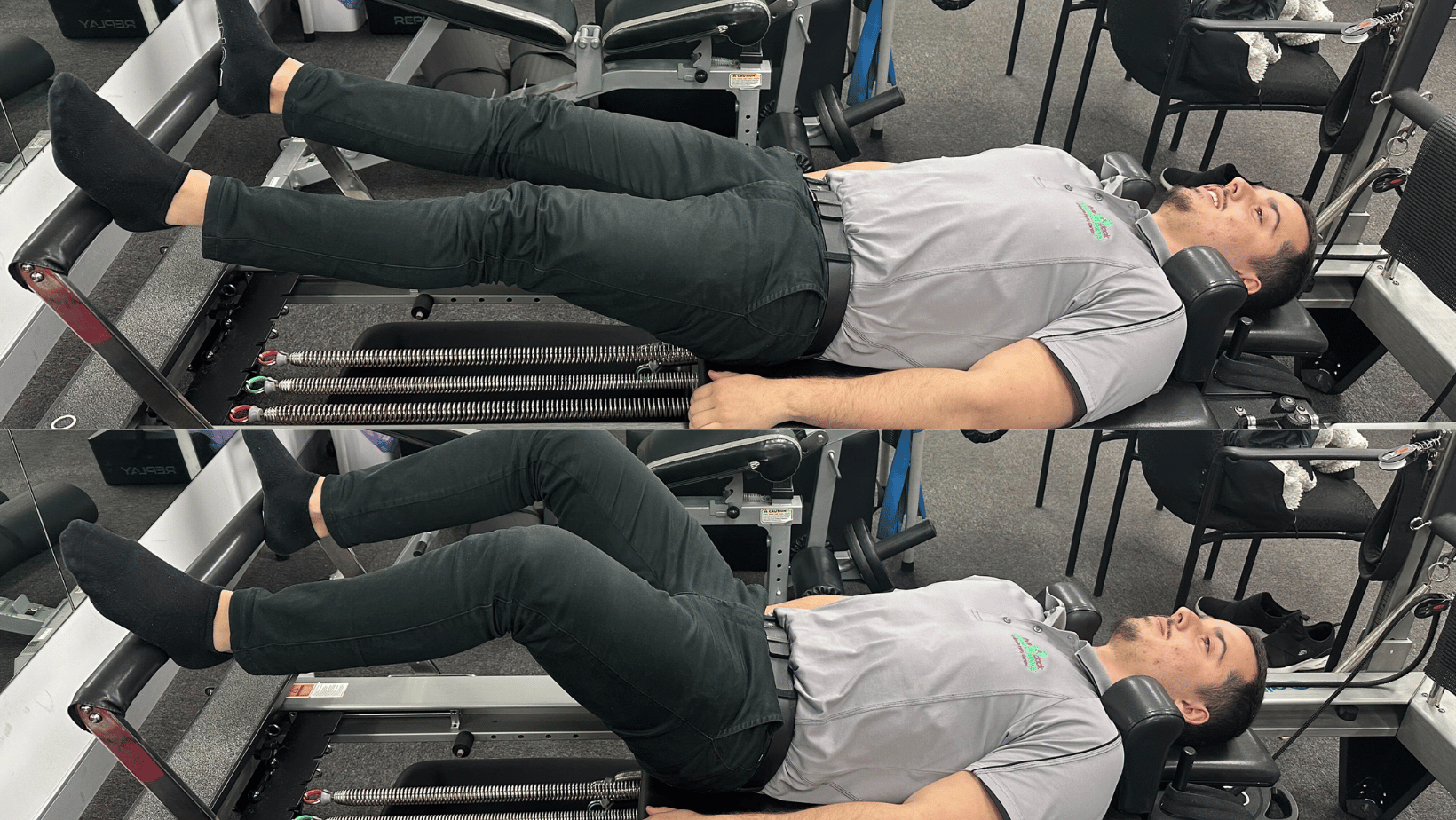
Leg press on the reformer
Aim: Improve quadricep and gluteal activation
How: Lying in supine on the reformer with feet placed on the foot bar, straighten out your knees working your quads and glutes. Ensure that your knees track in line with your second toe and don’t buckle in activating your gluteus medius. Adjust springs for more or less resistance.
Disc Load
Aim: Gait retraining exercise to normalise walking pattern
How: With one foot placed on a Dura Disc and the other foot in line, simply step up extending your knee placing weight through your heels activating your muscles. Hold for 3-5 seconds and then step down allowing your knee to bend. Repeat 10 times.

If you or someone you care for has an injury, a flare up, requires some rehabilitation or experiences an increase in pain, give the clinic a call on 9713 2455 or book online.