Have you started walking or running as a result of lockdown? Have you perhaps overdone it or noticed your shoes aren’t great and started to feel pain in the back of your heel around your Achilles tendon?
If so you are not alone. With the increase in outdoor exercise due to lockdown, this year we have found a spike in cases of foot and heel injuries, in particular a condition known as Achilles Tendinopathy. Although we do typically see this issue year-round with different segments of the population, as available exercise has changed with gyms closed and group exercise paused, there has been an upsurge in people walking and running as their main form of exercise, which can put an increase in stress on the Achilles Tendon.
The Achilles tendon is the combined tendon of the gastrocnemius and soleus muscles (calf muscles) and is the strongest tendon in the body (O’Brien, 2005). Through this tendon these muscles are able to point your toes moving your ankle and in effect provide “push off” when you walk and run transmitting all the force through your body.
Commonly, the Achilles tendon is prone to injury when exposed to activities involving repetitive high loads such as running, jumping and sudden acceleration or deceleration. However, it can also be overloaded following an increase in weightbearing activities such as walking. Overload of this tendon (its working too hard) can make physical changes to the actual tendons appearance giving rise to Achilles tendinopathy.
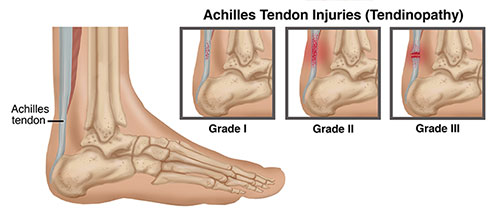
Image Ref: https://www.choosept.com/symptomsconditionsdetail/physical-therapy-guide-to-achilles-tendon-injuries-tendinopathy
Pathology
Achilles tendinopathy can be classified as a midsubstance (2-6cm proximal to the insertion) or an insertional (within 2cm of the insertion) tendinopathy with the main difference being the location of pain. Mid substance injuries are the most common among both active and inactive people.
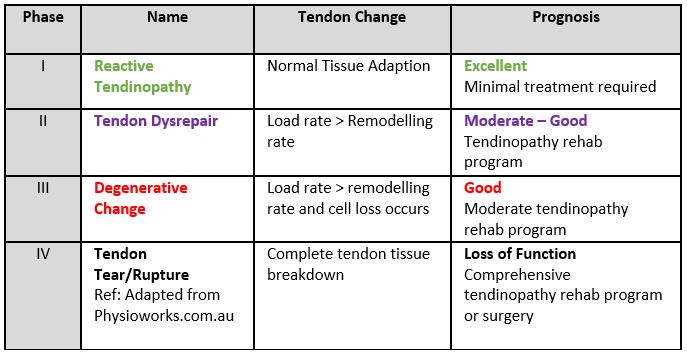
Injury to the tendon occurs along a continuum and can be classified into different stages. Based on the changes and distribution of disorganisation within the tendon, the stages are described as “reactive tendinopathy”, “tendon dysrepair”, and a “degenerative tendon”. The tendon can change on this continuum as a response to increasing or reducing load to the tendon. This is important during recovery as our physiotherapists will provide advice on activity load according to the stage of injury in order to promote tendon healing through optimal loading.
What is load?
Load can be thought of as how much capacity or tolerance a muscle or tendon has in relation to activity. We know that tendon’s are sensitive to load. This means that with activity, the tendons cells absorb this load and produce biochemicals that lead to changes in the tendon, sometimes these are positive changes allowing adaptation providing the tendon can withstand the graded changes over time, but when too much load occurs, and the tendon cannot cope with the demands placed on it, injury or symptoms can occur and can even lead to degenerative changes.
What Causes Achilles Tendinopathy
Multiple intrinsic and extrinsic factors can influence the tendon’s response to the subjected load. The Achilles tendon is subjected to the highest loads in the body, with tensile loads up to ten times our body weight during running, jumping, hopping, and skipping (O’Brien, 2005).
Therefore, the tendon’s capacity for load is specifically related to the individual’s makeup and their activities. The primary mechanism for tendinopathy is overload of the tendon combined with compressive overload proposed to cause the tendinopathic process within the tissue. Essentially a failed healing response occurs leading to increased susceptibility to damage (Longo et al. 2009, Brukner and Khan, 2017, Cook and Purdam et al. 2012).
Risk Factors:
- Increased distance, speed and frequency of training/activity
- Increased BMI, adiposity, hypercholestremia, diabetes mellitus
- Previous tendinopathy and genetic predisposition
- Recent change in footwear or training surface
- Weakness and poor endurance of ankle plantarflexors & knee flexors (Calf and hamstring muscles)
- Altered biomechanics/muscle activation along the kinetic chain including poor gluteal and core muscle activation
How are symptoms described?
Patients usually report pain at the beginning of an activity, which can then reduce during the actual activity as they “warm up” and often symptoms can worsen following the event/activity. The tendon will often be described as stiff and painful and a loss of strength in the affected area is typically experienced. Movements involving plantarflexion (pointing toes) and push off during the gait cycle typically cause pain, and symptoms can also be present during the night or on first steps in the morning.
The Achilles itself may be tender, red, warm, or present with a swollen lump on the actual tendon. Pain can vary significantly between patients depending upon on where they are on the continuum described earlier and their individual exercise load and capacity or tolerance levels.
Diagnosis and Examination
Physiotherapy examination begins with comprehensive questioning and physical assessment. To get the best result with physiotherapy it is important to understand the your activity levels, your aggravating factors, changes in training (distance, speed and frequency) or footwear changes, the activity levels that you wish to get to with our rehabilitation (your goals) and your typical daily load capacity. Your load capacity is impacted by the incidental things that you do domestically, at work, your load during hobbies and also your load with relation to your general exercise. Understanding the impact that previous injuries can have can also be vital. In our examination we aim to understand how and why your tendon has become overloaded and once diagnosed we typically prescribe a treatment plan so we can help you get back to your goals.
In our physical examination will often see:
- Thickening or enlargement of the Achilles tendon itself, and sometime even swelling along the tendon or at the back of the heel
- Calcaneal spurs may be present (especially in insertional tendinopathy and calcific tendinopathy)
- Tenderness through the midportion of the tendon in mid-substance tendinopathy or at the calcaneal insertion (heel bone) with insertional tendinopathy
- Potential limitation in range of motion on dorsiflexion testing (toes towards your head) as the tendon is stretched
- Pain noted when testing calf strength raising on your toes either on two legs or one
- Potential wasting of other muscles like your quads, gluteals, gastrocnemius or soleus
- A limp may be present
- Poor gluteal stability and activation
- Altered foot posture
Treatment and evidence:
After assessment in our clinic, treatment will begin immediately. This may firstly involve some soft tissue work to help reduce excessive tightness when there is muscle dysfunction, and manual therapy or mobilisation techniques when joint hypomobility is affecting normal movement. Our Physiotherapists will also help in the management of tendon loading, through providing education, exercise prescription and monitoring. Education and exercise is vital for effective treatment in order to progressively load the muscle tendon unit. The ideal exercise program will allow the tendon to develop tolerance to load, as opposed to an actual change in the tendon structure. An initial reduction in aggravating loads will be advised to ease symptoms, followed by a progressive increase in load, to improve tendon load capacity. Activity and load tolerance is a constant factor that is educated on during the recovery of Achilles tendinopathy. Incidental load is an important factor to consider. For example, being on your feet for work, then popping past the shops before doing your formal exercise may prefatigued the muscles, so that when you then set out for that walk you have exceeded your muscle-tendon units load capacity thus bringing on symptoms, tightness, and compensation strategies. Symptoms may also be experienced the day after this spike in load, typically presenting as morning pain and stiffness. So, the time-of-day exercise is performed can be an incredibly important factor with regards to recovery but so can the total amount of daily accumulated load. Pacing activity (doing the activity, but with breaks) can sometimes be a strategy used to keep symptoms in check for patients that lack endurance, e.g., a 20-minute walk 2 times a day instead of one 40 minute walk, as this way rest and recovery can occur. However, this still contributes to total load which needs to be considered.

Exercise
For an irritable tendon, isometric exercises can help to reduce pain, whilst allowing a load stimulus to occur but is not a long-term strategy. Bradford et al. (2021) reports that 5 reps of 40 second isometric holds can produce a 50% reduction in Achilles tendon pain. As the affected patient progresses through rehabilitation, slow heavy strengthening, concentric and eccentric loading, and sport specific loading if applicable should be included. Weaknesses of the kinetic chain will be identified and addressed, to improve outcome and load capacity of the entire kinetic chain, whilst also reducing the risk of re-injury. Patients with Achilles tendinopathy were found to be 30% weaker at the hips (Habets et al, 2016), so this needs to be assessed and addressed. As an adjunct to exercise along the course of treatment, different physio treatment tools may be utilised, including massage, ice, heel raises and taping to assist with symptom control (Brukner and Khan, 2017). Ultimately, the tendon must be loaded, and complete rest is discouraged (Cook et al. 2012) as this only settles symptoms and does not increase the tendon’s ability to handle loading. If a patient were to rest completely, they may experience improvement with simple ADL’s, but symptoms return as soon as they return to exercise.
In the late 1990’s, eccentric exercises were considered the gold standard, involving isolated slow-lengthening muscle contractions (Alfredson et al. 1998). Although, more recently this method has been compared to other types of muscle contraction and research has shown that not all patients respond positively to this loading, specifically sedentary patients (Sayana et al. 2007). Results from Beyer et al. 2015 showed that both traditional eccentric loading and heavy slow resistance exercises improve function and reduce pain in both the short and long term (1 year). Heavy slow resistance exercise has been suggested as the preferred type of muscle contraction. This contraction type addresses weakness in concentric strength and the associated muscle replicate’s everyday function and has shown greater patient satisfaction (Malliaras et al. 2013 and Beyer et al. 2015). To achieve the best outcome exercise needs to be targeted to the individual, the stage of pathology and patient’s functional demands and goals (Malliaras et al. 2013). Being experts in exercise prescription and musculoskeletal assessment, this evidence supports that physiotherapists manage Achilles tendinopathy.

Importantly during rehabilitation our physio’s set objective markers that link to functional tasks or goals that our patients wish to achieve. For example, without hitting adequate calf strength markers, and having poor gluteal stability when on one leg, hopping and running cannot typically be progressed to safely with good biomechanics. It is important that these objective physio markers are reached to minimize the risk of re-injury, and as a clinic that is our goal, to not only reduce our patient’s pain, but help them achieve their goals and reduce the risk of re-injury or a return of symptoms.
Conclusion
Achilles Tendinopathy is a common condition seen in different populations of the community. Professional and weekend athletes can suffer from Achilles tendinopathy, but it’s also a common overuse injury in people not involved in sport. Understanding the pathology, load capacity and biomechanics is incredibly important to get a good outcome as these factors will help determine how exercise and activity is progressed so that an improvement in function can be achieved. It is important to note that symptomatic recovery does not equate to functional recovery, and without the right strength gains the recurrence rate can be as high a 27% (Gajhede-Knudsen et al, 2013). It is important that on discharge strength programs continue to prevent further issues arising. Physiotherapists are best placed to treat this condition.

