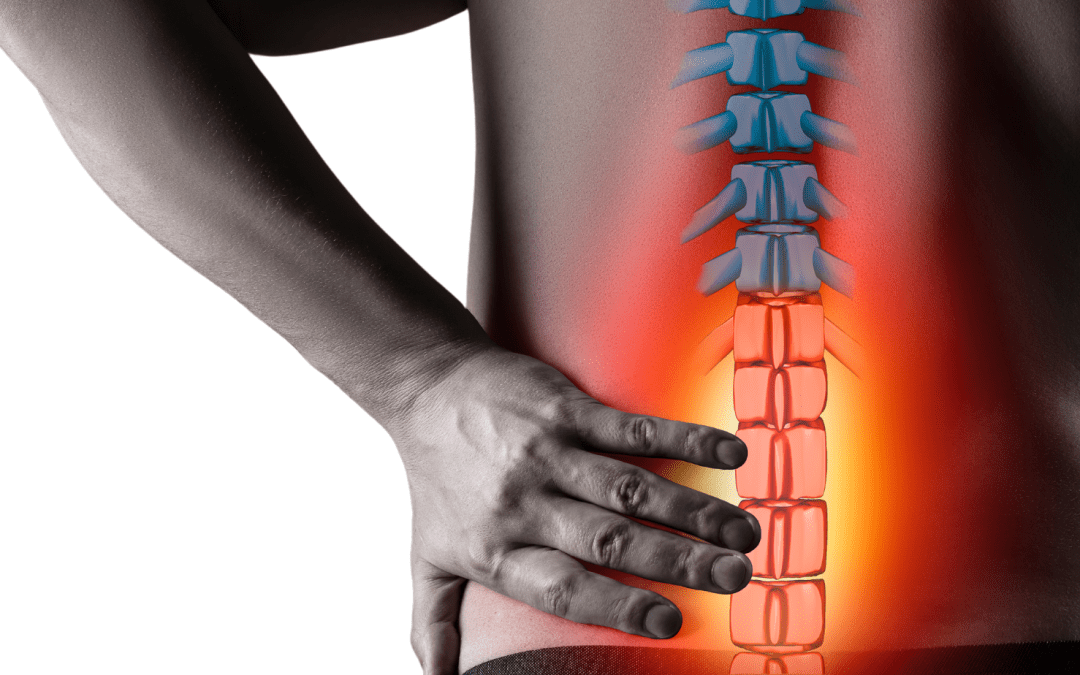
Sciatica” is a term that refers to pain that runs along the course of the sciatic nerve. This nerve branch originates from L4-S2 nerve roots in the lower back, running through the hips and buttocks and down through the legs (Teles et al., 2020). Sciatica is not a diagnosis, but a description of the symptoms.
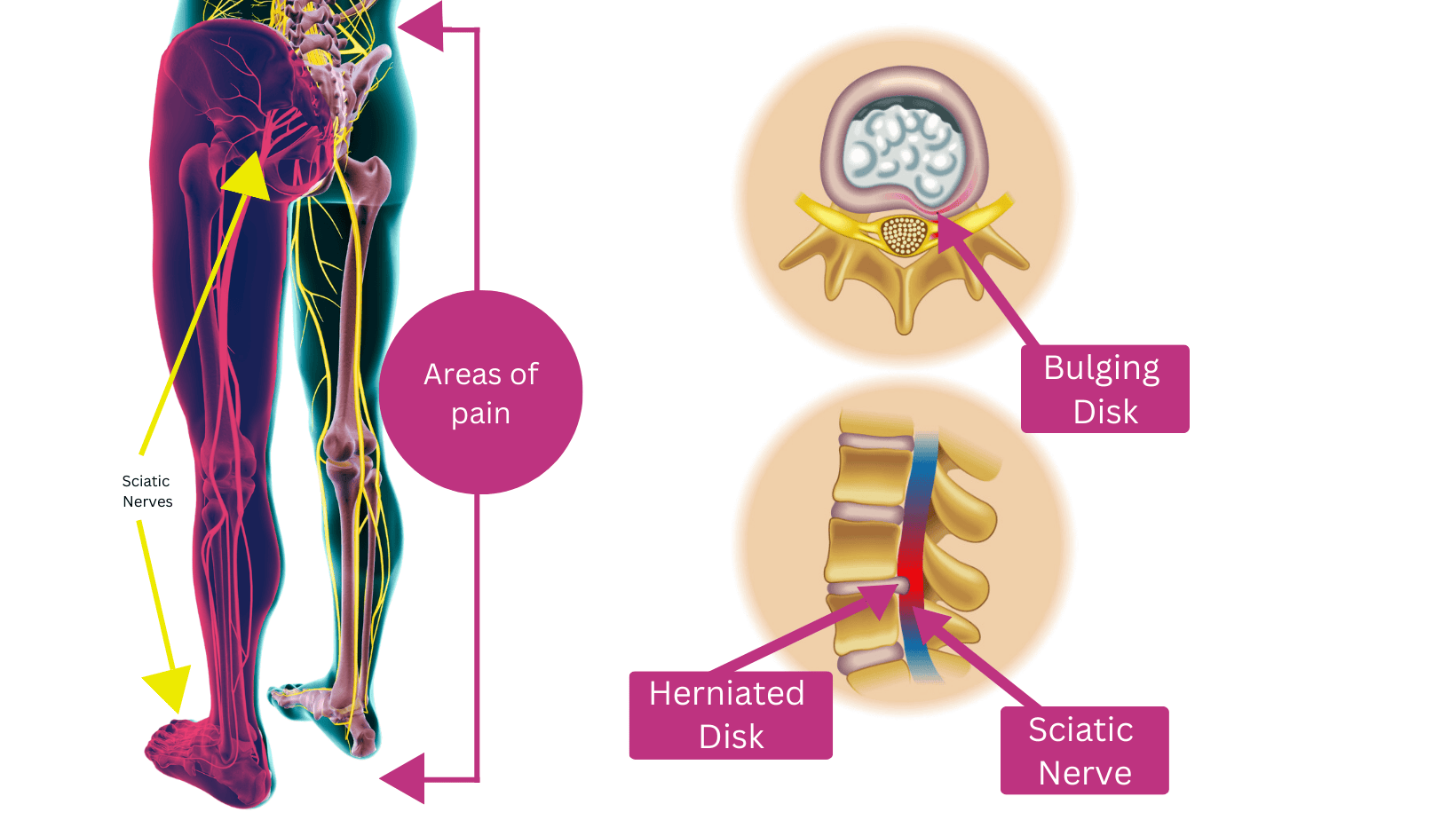
Irritation or compression of the sciatic nerve can lead to radiating pain, sometimes extending to the foot, with symptoms like shooting or burning pain in the glutes and thigh, along with pins and needles, weakness, or numbness. Although sciatica itself is not a standalone condition, it signifies an underlying issue with the sciatic nerve, often caused by herniated discs or spinal stenosis (Maitra et al., 2020; Williams et al., 2022).
Causes of Sciatica
Herniated Disc: The most frequent cause, where a disc in the spine protrudes and presses on the sciatic nerve.
Spinal Stenosis: Narrowing of the spinal canal that compresses the nerve roots.
Degenerative Disc Disease: Breakdown of discs leading to nerve irritation.
Spondylolisthesis: A condition where a vertebra slips out of place and compresses the nerve.
Piriformis Syndrome: A muscle in the buttock area that irritates the sciatic nerve if it becomes tight or inflamed.
Risk Factors
Age: The risk increases with age due to degenerative changes in the spine.
Occupation: Jobs that involve heavy lifting, prolonged sitting, or twisting motions can contribute to sciatica.
Obesity: Excess weight can place additional stress on the spine and sciatic nerve.
Sedentary Lifestyle: Lack of exercise can weaken the muscles that support the spine.
Diabetes: Can increase the risk of nerve damage, including the sciatic nerve.
Findings on Assessment
Confirmation of the presence of sciatica can be determined through a combination of a subjective assessment, clinical examination, and imaging techniques. A physiotherapist will first assess any areas of restricted mobility or muscle tightness, as well as identify any muscle strength deficits, particularly in the core and gluteal muscles (Miller et al., 2022). Symptoms can typically be reproduced on palpation of the lumbar nerve roots or through specific trigger points in the hip, depending on where the nerve is being irritated, which often leads to pain radiating down the course of the sciatic nerve (Harris & Smith, 2021). A comprehensive clinical examination is crucial, as it helps to differentiate sciatica from other conditions that may present with similar symptoms, such as lumbar radiculopathy (Johnson et al., 2023). If necessary, imaging such as an MRI or CT scan can then be utilised to confirm the source of the issue, providing valuable insights into the presence of herniated discs or spinal stenosis that may be contributing to nerve compression (Lee & Nguyen, 2022). This multifaceted approach ensures a more accurate diagnosis and facilitates the development of a tailored treatment plan. Imaging is not always necessary or helpful as physiotherapists treat the patient and not the scan (Brinjikji et al., 2015). Current global guidelines only recommend imaging in cases where serious pathology or radiculopathy is suspected, or if no improvement is seen after 4 weeks of Physiotherapy.

Physiotherapy Management of Sciatica
Managing sciatica typically begins with a combination of manual therapy, exercise therapy, and activity modification. Manual therapy, including joint mobilisations and trigger point release; helps alleviate muscle tightness and joint stiffness that compress the sciatic nerve, providing temporary symptomatic relief. However, this approach is most effective when combined with exercise therapy. In the early stages of rehabilitation certain exercises aim to get our patients moving again and provide relief, whilst other exercises help restore muscle activation patterns including gluteal and core control. As progress is made, our physiotherapists will start to focus on strength, and progress motor control and endurance exercises. This progression through rehabilitation is essential to getting patients back to achieving their goals whether it be work/sport/life and preventing recurrences. Depending on the patient’s goals we will often guide this process and empower them by taking our patients to the gym or leading them through a Clinical Pilates-based exercise program. Dove et al (2023) found that physiotherapy is particularly effective for long-term pain relief and disability management.
Additionally, activity modification is crucial to overcoming barriers to recovery as specific movements or postures can hinder progress and increase injury risk. Physiotherapists provide individualised advice on which activities to reduce or modify until symptoms reduce and function improves. While injections may offer temporary relief in severe cases, they do not address the underlying causes and should be used judiciously. Surgery is considered a last resort for persistent cases where conservative treatments have failed, aimed at relieving pressure on the sciatic nerve. Together, these strategies emphasize a comprehensive approach to managing sciatica effectively.
Evidence
A systematic review and meta-analysis by Dove et al. (2023) assessed the effectiveness of physiotherapy in treating sciatica, concluding that physiotherapy significantly outperformed minimal interventions for long-term pain relief and improved disability outcomes. Physiotherapy encompasses several benefits, including enhanced mobility, better posture, individualized treatment plans, and preventive measures (Johnson et al., 2023). By employing targeted exercises and manual therapy, physiotherapy not only reduces inflammation and improves blood flow but also accelerates healing. Additionally, physiotherapists educate patients on body mechanics and ergonomics, equipping them to manage their condition effectively and prevent recurrences.
A 2022 study highlighted the effectiveness of a structured Pilates program for sciatica patients, reporting significant pain reduction and improved functional mobility after 12 weeks (Smith et al., 2022). Active rehabilitation strategies, such as Pilates, are crucial in managing sciatica effectively.
Athletes, particularly runners and cyclists, often experience sciatica due to overuse injuries, technique issues, load management and poor equipment set up altering posture. Research indicates that around 75% of athletes experience significant pain relief and functional improvement within 8 weeks of starting physiotherapy (Australian Journal of Physiotherapy, 2022). Additionally, 60% of athletes returned to their pre-injury competition levels within 6 months, although 30% experienced recurring symptoms (Journal of Musculoskeletal & Neuronal Interactions, 2019). Studies on the socio-economic impacts of sciatica reveal increased absenteeism, reduced physical activity, and negative effects on mental well-being (Jones et al., 2020). Notably, Liu et al. (2023) found that non-surgical treatments, such as physiotherapy, were superior to surgical options in managing sciatica symptoms, emphasizing the importance of conservative treatment strategies. Collectively, these findings suggest prioritizing physiotherapy and non-surgical interventions can lead to better outcomes for those suffering from sciatica.
Exercise
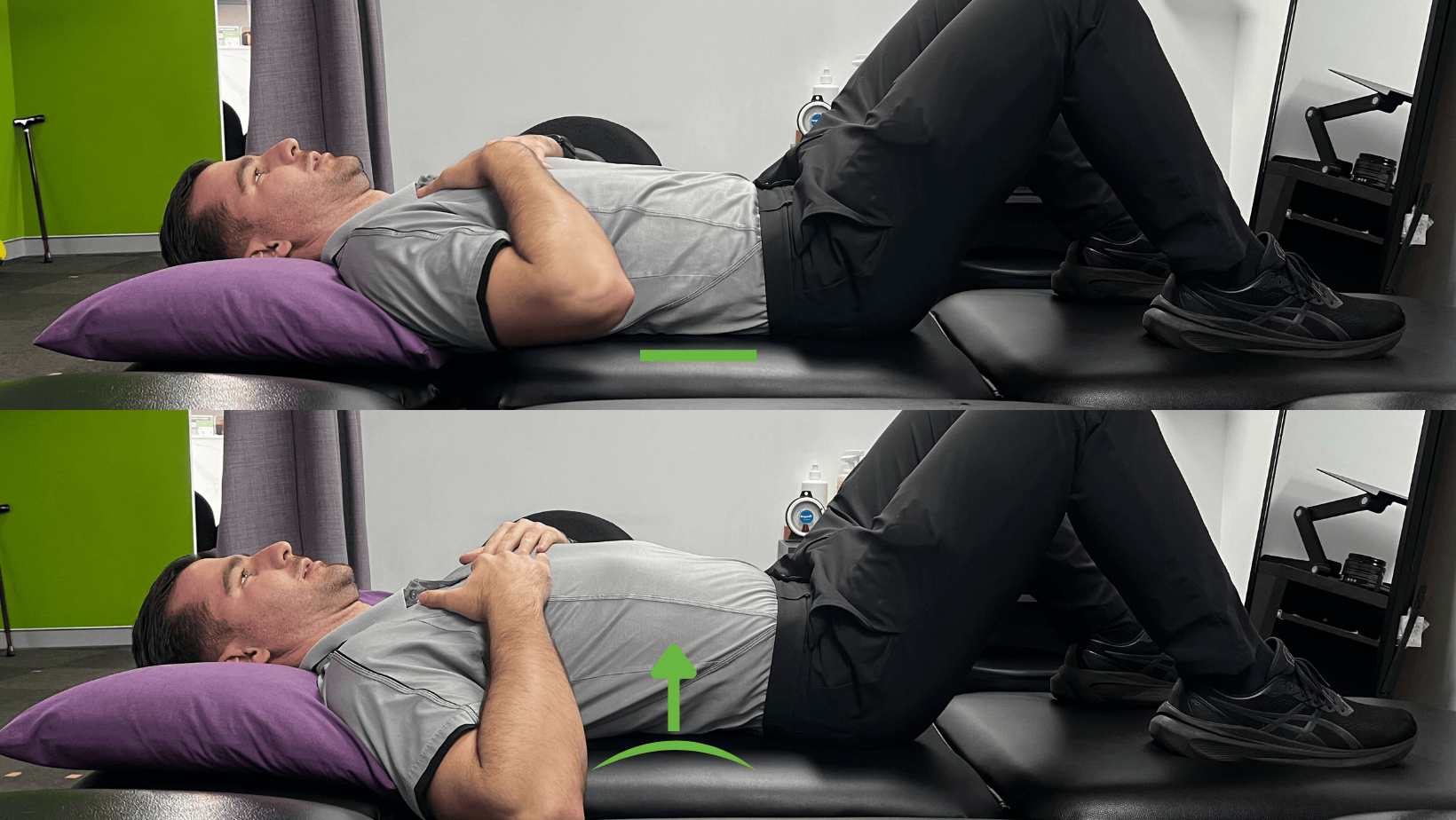
Pelvic Tilts
Aim: Improve core activation, reduce lumbar spine stiffness.
How: Lying on your back, bend your knees so your feet are flat on the floor/bed. Tilt your pelvis, so that your core engages & your low back flattens. Think about tilting your belt buckle towards your chin. Hold for 3 seconds, then relax. Perform 10 times.
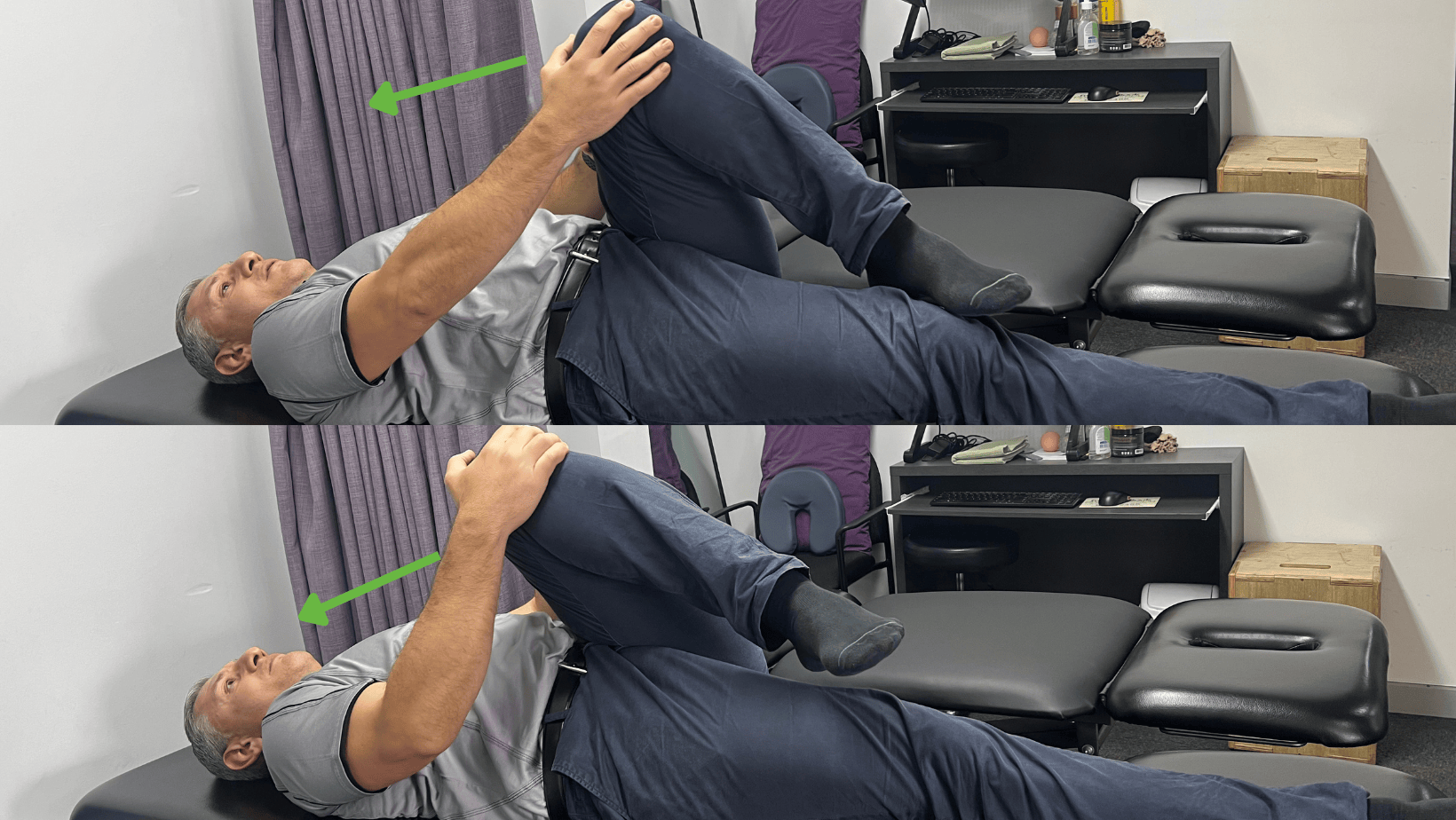
Piriformus Stretch
Aim: Improve lower back mobility stretching out the piriformus and gluteals
How: Lie supine. Pull one knee towards the opposite shoulder until a stretch is felt in the gluteal region. Hold for 20-30 seconds.
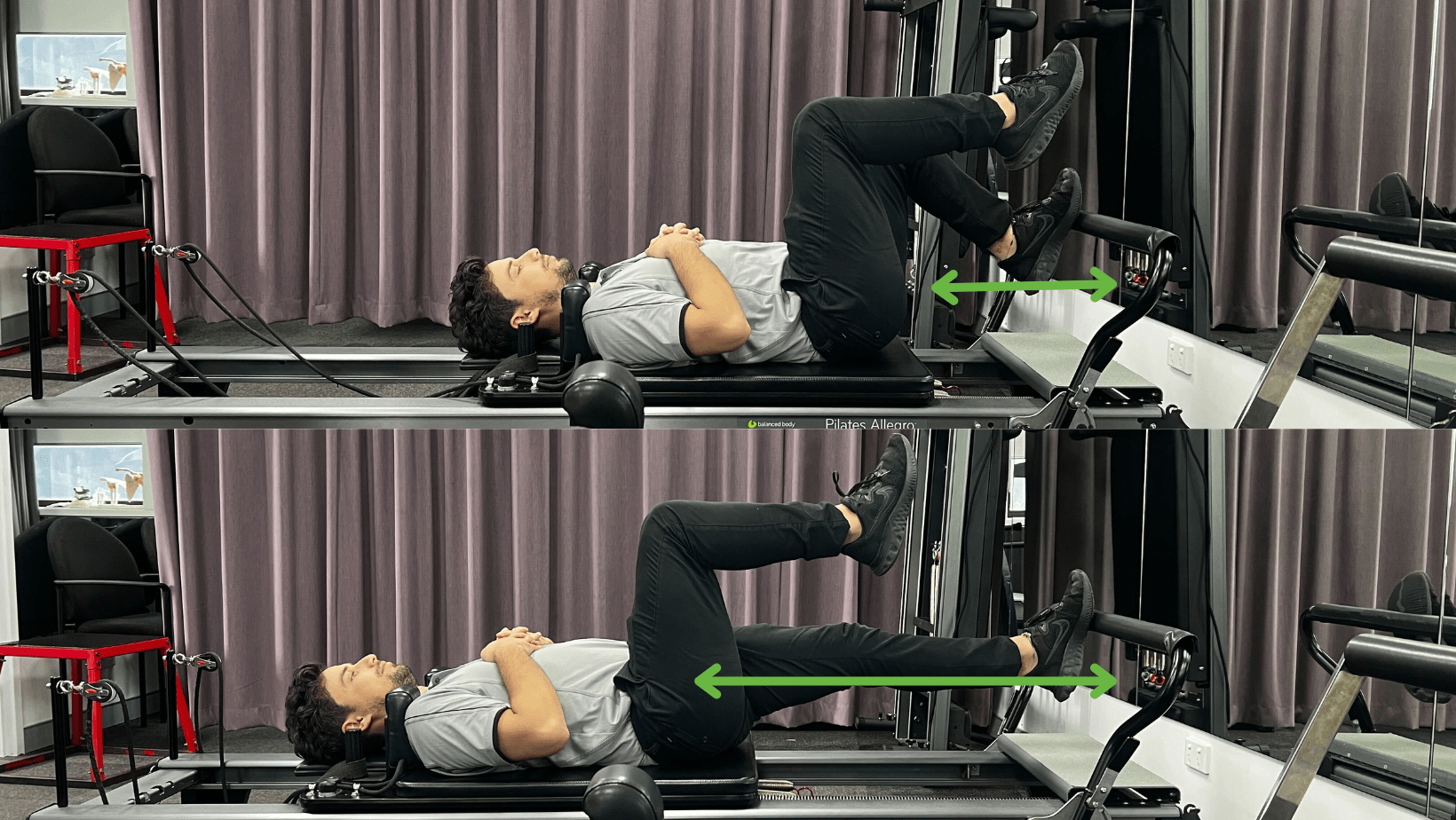
Single Legged press on the Reformer
Aim: Improve core, gluteal and quadricep activation
How: Lying in supine on the reformer with one foot in table top and one foot placed on the foot bar, straighten your leg. Ensure that your knee tracks in line with your second toe and don’t buckle in activating your gluteus medius. Adjust springs for more or less resistance.
If you or someone you care for has an injury, a flare up, requires some rehabilitation or experiences an increase in pain, give the clinic a call on 9713 2455 or book online.