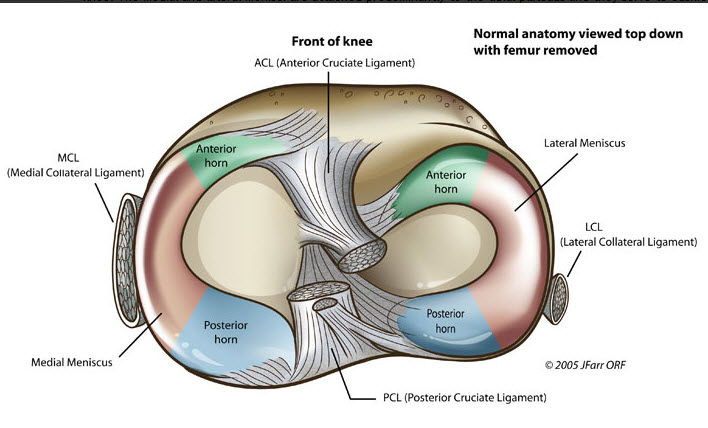
The medial and lateral menisci are two C-shaped fibrocartilaginous structures located on the top of the tibia. They act as a shock absorber, stabiliser and are an attachment site for tendons, muscles and ligaments.
Acute meniscal tears typically occur through twisting, loading, hyperextension or direct trauma to the knee. They have a prevalence of 12-14% (Valdez et al.,2021). These meniscal tears can occur in isolation or in combination with a ligamentous injury like an ACL tear. Tears can also occur through “wear and tear” over time, which are called degenerative tears. This is often associated with ageing, repetitive stress like kneeling or squatting or underlying conditions such as osteoarthritis. These degenerative tears have a peak onset age in men of 41 to 50 years, while in females, it is 61 to 70 (Luvsannyam et al, 2022).
Signs and Symptoms
- Pain with weightbearing – particularly along the joint line of the knee
- Swelling in the knee joint (commonly delayed after injury)
- Restricted knee movement (Difficulty bending or straightening and can include ‘locking’ sensation)
Risk Factors
- Involvement in sports requiring running, jumping, changing direction or pivoting
- History of previous knee injury – The evidence shows that individuals who experience injuries such as ACL tears have an increased risk of meniscus tears in the future.
- Age – more common in the older population due to the degenerative changes in cartilage
- Occupational activities: Frequent squatting, kneeling or stair climbing
- Poor biomechanics – including lower kinetic chain dysfunction
- Weight – With increased bodyweight, the meniscus undertakes more load and stress which can contribute to degeneration and tears.
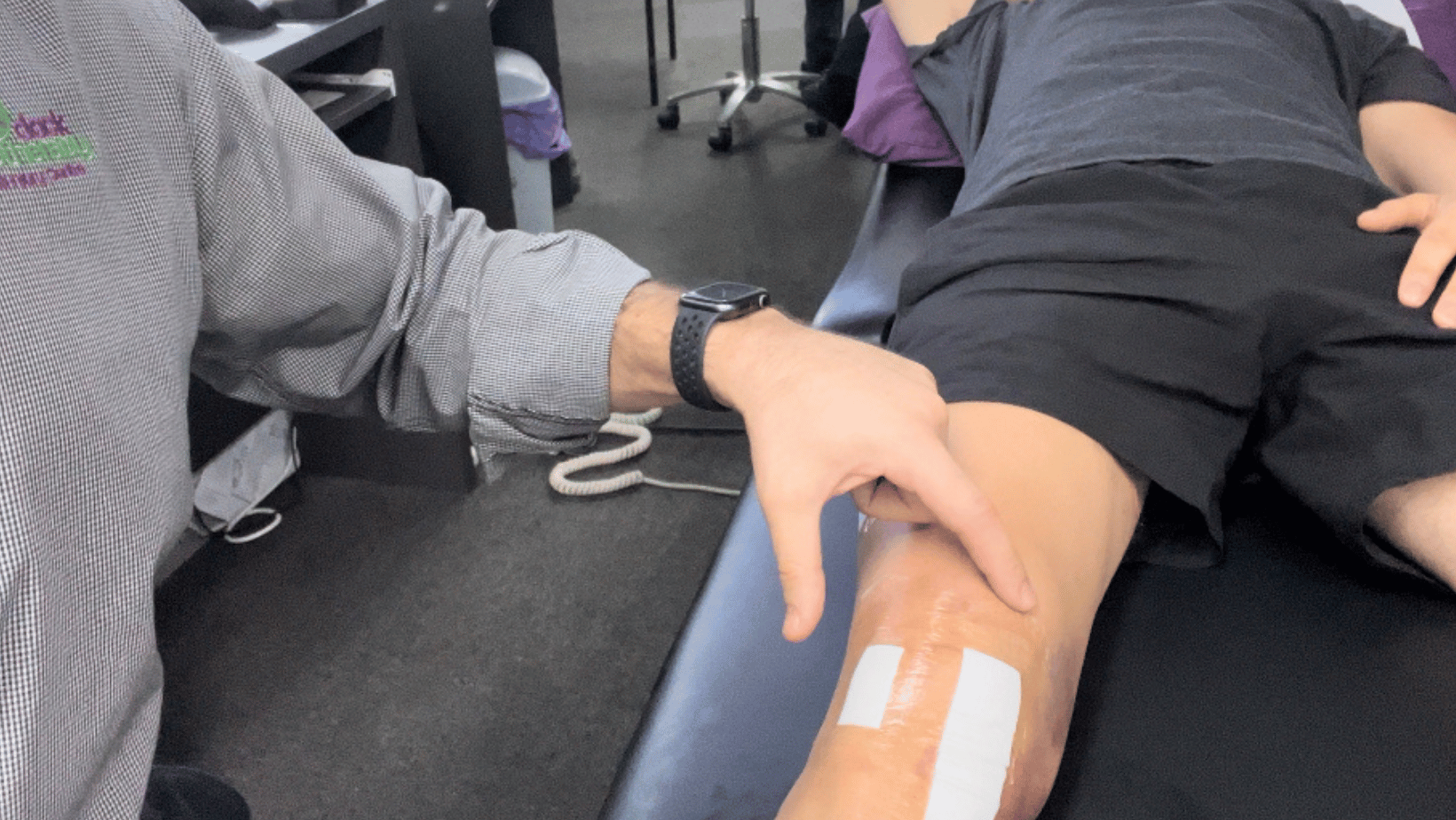
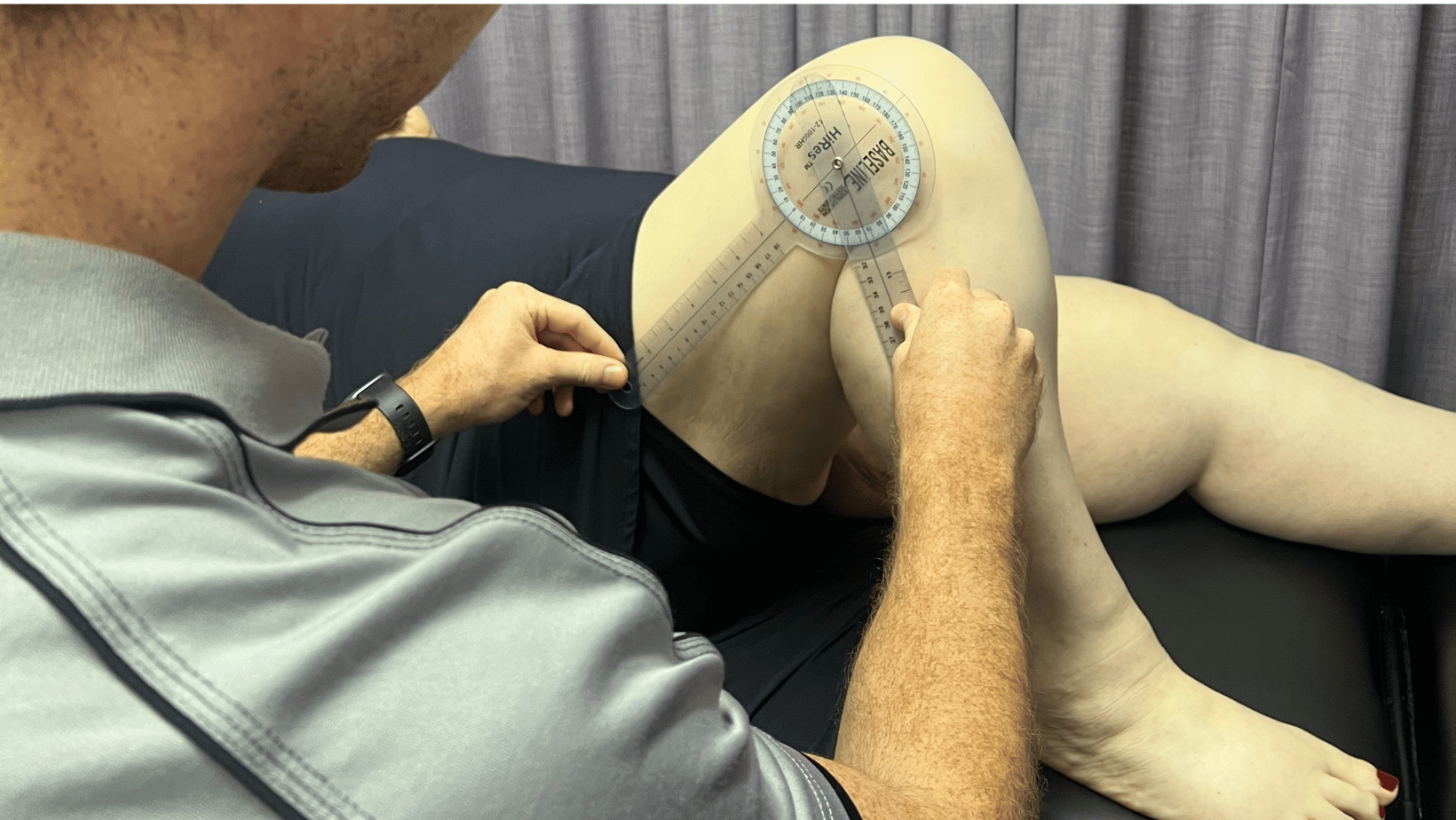
Diagnosis/Assessment
- Knee joint swelling/effusion present
- Reduce knee joint range of motion
- Inability to fully straighten knee
- Positive McMurray’s test (Pain +/- click or clunk)
- Tibiofemoral joint line tenderness
- Inability to squat or “duck walk”
- MRI can assist alongside clinical diagnosis.
- Lower limb biomechanics, muscle activation patterns and strength are also assessed
Treatment – Which Approach Should We Take In Managing These Injuries?
Depending on the type and severity of a meniscal tear, they may be treated with either a conservative or surgical approach.
Conservative Approach
- Symptoms develop 24 – 48 hours post injury
- Minimal injury or unable to recall injury
- Able to weight bear
- Minimal swelling
- Full ROM with pain only at end of range
- Pain on McMurray’s test at end of range flexion only
- Previous history of rapid recovery from similar injury
- Early degenerative changes on x-ray

Surgical Approach
- Severe twisting injury, unable to continue playing
- Locked knee or severely restricted ROM
- Positive McMurray’s test- “clunk”
- Pain on early range flexion on McMurray’s test
- Presence of ACL tear
- Little improvement after 3-4 weeks of conservative treatment
- Type, location, severity or size of tear
Current evidence
A systematic review by Fernandez-Matias et al, 2023, found that in the management of degenerative meniscal tears at 5-year follow-up, knee function was the same when comparing effectiveness of exercise alone versus exercises with an arthroscopic partial meniscectomy. This means that surgery had no additional benefit and validates that a rehabilitation exercise program compiled by a physiotherapist can be just as effective.
When comparing surgery versus conservative management even for acute or unstable meniscal tears in a non-osteoarthritic knee, Abram, 2020, suggested that surgical treatment should not be considered as the first line intervention when it comes to management of these injuries. Brukner (2012) suggests, a physiotherapy approach should be undertaken for 3-4 weeks following meniscal tears, however failure with conservative management would require surgical intervention.
Why is physio important?
Meniscal injuries can cause accelerated wearing of cartilage and lead to early onset of osteoarthritis in the knee (Jarraya et al, 2017). Therefore, management should be sought in the early stages to reduce the pressure on the meniscus as well as secondary compensations.
Meniscal tear patients with higher levels of leg strength had less pain, less difficulty completing daily tasks and had improved mobility compared to those with reduced strength (Luc-Harkey et al, 2018). This shows the importance of a strengthening program to address the supporting muscles around the meniscus.
Early physio management after meniscal injury helps to normalise the injured persons gait and improve muscle activation patterns, improving their chance of non-surgical management. This typically leads to less pain, less dysfunction and a better outcome with an earlier return to ADL’s, sport and normal function.
Exercise
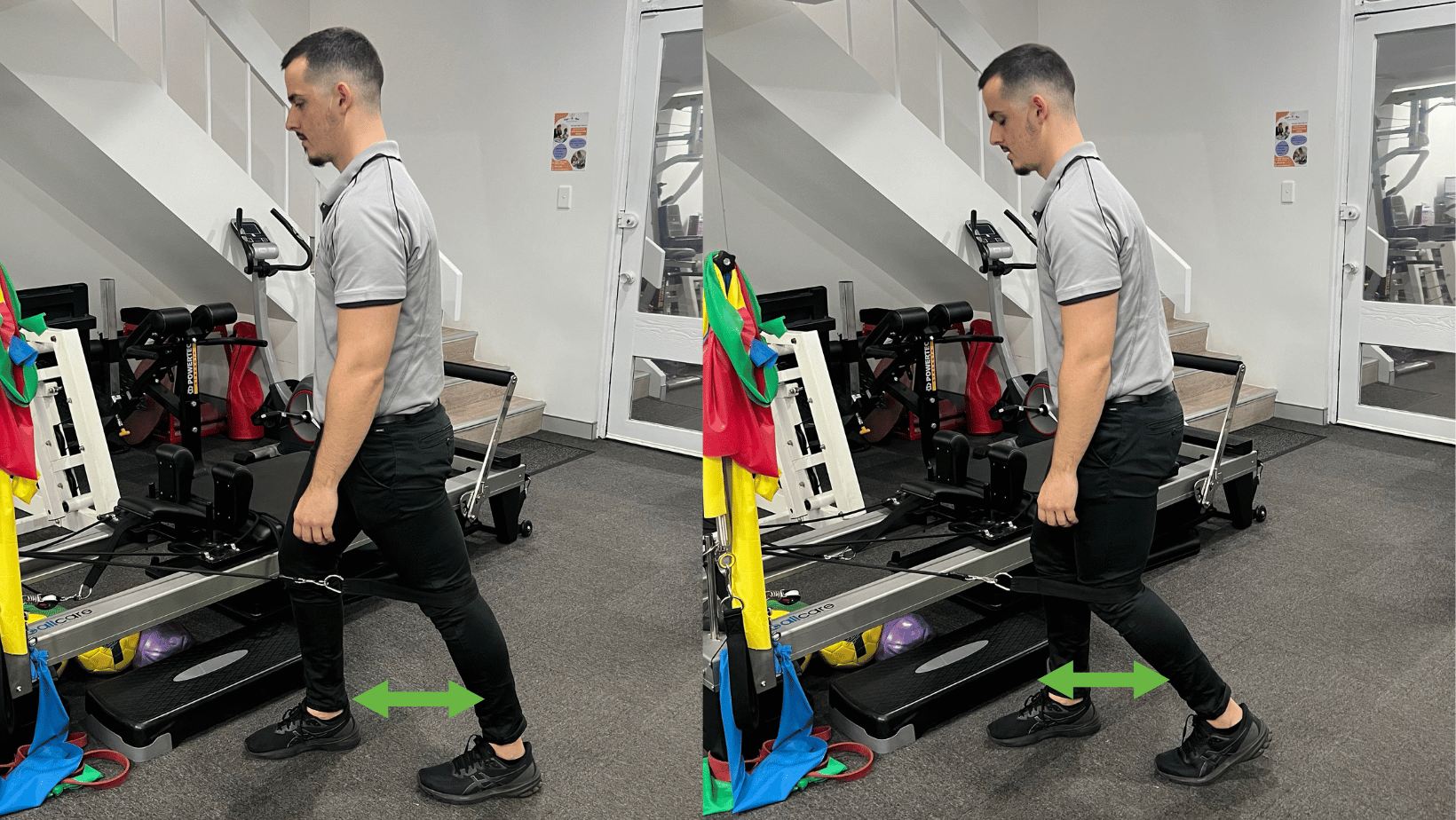
TKE using the Reformer
Aim: Improve knee extension movement and improve walking gait. Important in the early stage of rehab when you can’t extend your knee.
How: Step through the loop of the strap of the Pilates reformer, placing it around your knee. Starting with a bent knee simply straighten out your knee, placing you heel on the ground using resistance from the springs of the reformer. This helps to get your knee straight. Hold for 3 -5 seconds. Repeat for reps and add springs if you need more resistance.
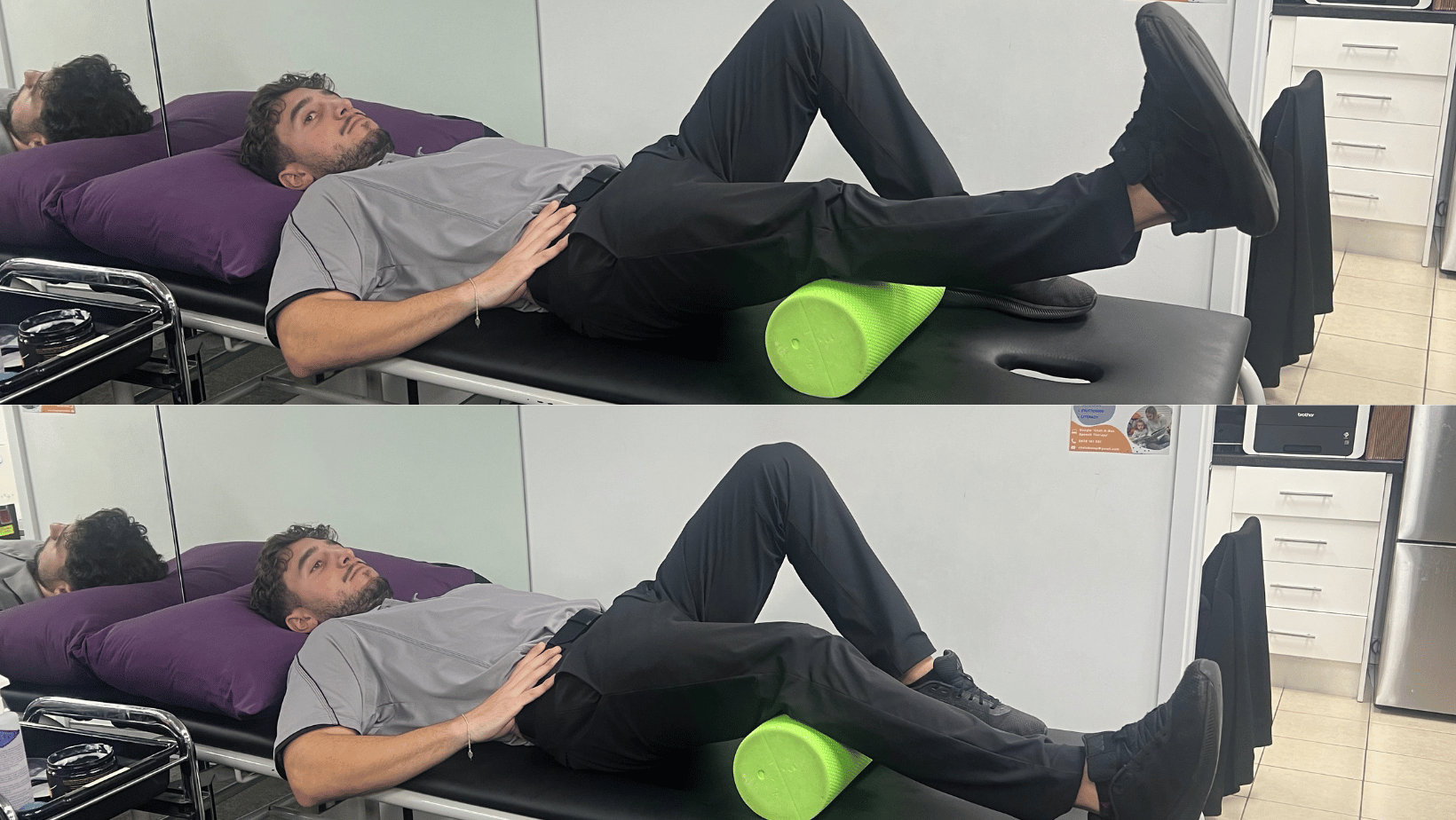
Inner Range Quad Exercises:
Aim: Improve VMO and Quad strength and activation
How: Lying on you back or sitting up tall with a foam roller under your knee crease simply straighten your leg out, tensing the muscle at the top for 5 seconds. Repeat for reps.
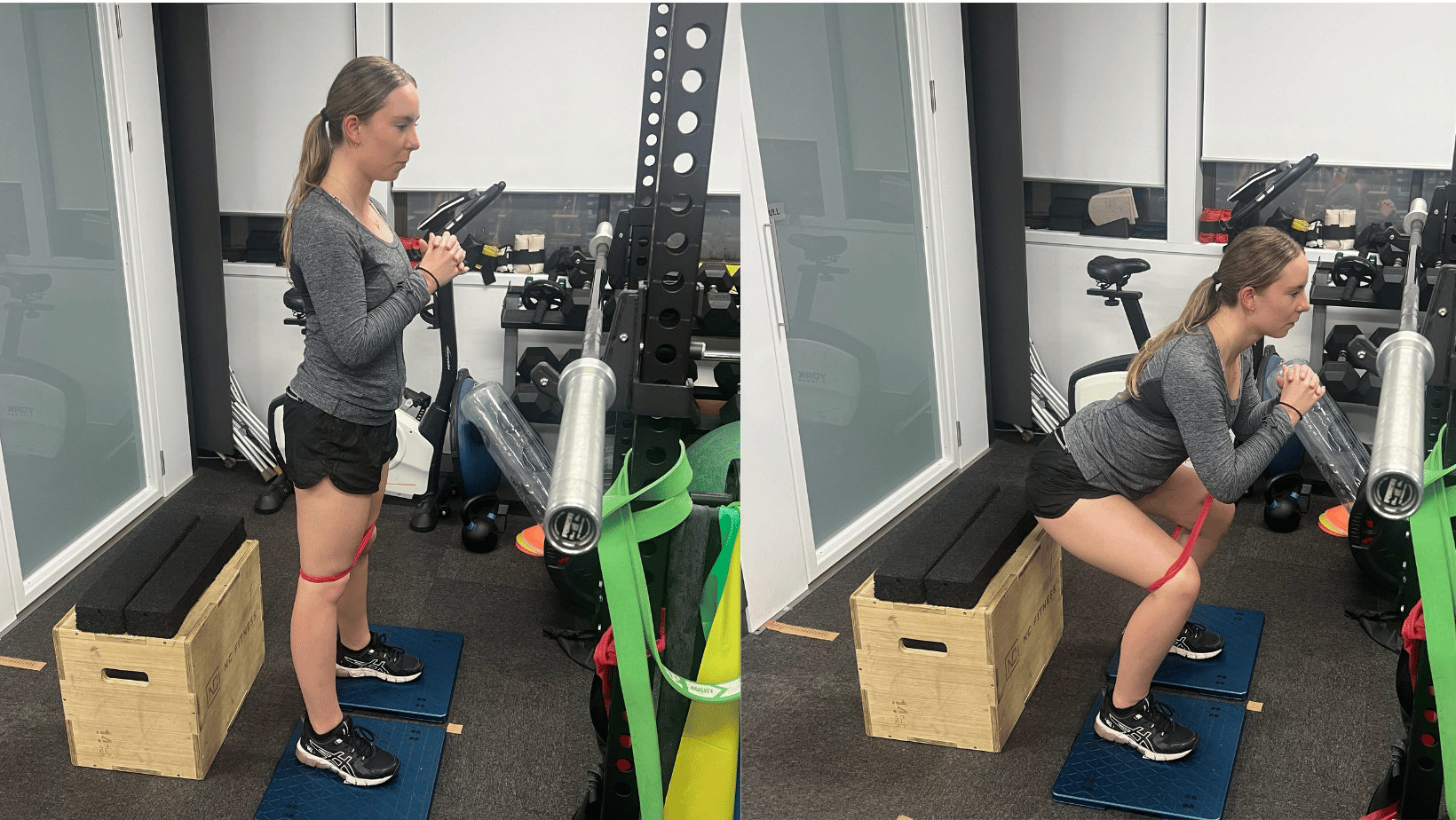
Squat using the AxIT
Aim: Improve lower limb strength, but also measure progress using the AxIT’s force plates
How: Standing on the force plates, sit back into a squat, pause and repeat for reps. Use a theraband around your knees to cue “pulling out” to ensure you engage your glute medius. The AxIT will measure your distribution of force and your strength. You will primarily work your Quadriceps, hamstrings, glutes and hip flexors.
If you or someone you care for has an injury, a flare up, requires some rehabilitation or experiences an increase in pain, give the clinic a call on 9713 2455 or book online.

